The University focuses research on coronavirus
Across the University of Leeds – from arts and humanities to fundamental science and engineering – teams are developing new ideas and redirecting existing research to help the world cope with the pandemic and its impact. Read on for details of a just a few of many examples of their work.

Effect of lockdown on air quality
Improvements in air quality in China during lockdown have been widely reported, but an analysis by the University of Leeds and the Southern University of Science and Technology in Shenzhen, China, reveals that the two pollutants most harmful to people were only slightly reduced or barely affected.
Their findings reveal PM2.5 – fine particles measuring less than 2.5 µm – had a modest reduction of 11% across China, and was not reduced in north-east China. These particles are the most harmful constituent of air pollution as they travel deep into the lungs and bloodstream and damage the lungs and heart.
Ozone (O3) at ground level can irritate breathing, affect lung function and worsen lung conditions such as asthma. The study found almost no change in Ozone concentrations as a result of the pandemic control measures.
Concentrations of Nitrogen Dioxide (NO2) did show improvements with a 27% decrease across China during the lockdown, and 50% decrease in Hubei province, the centre of the outbreak.
Ben Silver, a PhD researcher in the School of Earth and Environment at Leeds, said: "The modest improvement in air quality, despite very large reductions in emissions from some sources such as traffic, highlights the challenge facing China as it tries to further improve air quality."
The modest improvement in air quality, despite very large reductions in emissions from some sources such as traffic, highlights the challenge facing China as it tries to further improve air quality.
Understanding the impacts of COVID-19 control measures on air quality has been complicated by several compounding factors, including the Lunar New Year, which has a well-documented impact on air pollution in China and the rapidly changing air quality in China during recent years.
The study, published in the journal Environmental Research Letters, analysed five years of data from 1,600 air quality-monitoring stations in China to isolate the impact of the lockdown on air quality. The study controlled for and quantified the inter-annual trend, seasonal variation and effect of Lunar New Year on air quality in each province and city across China.
Ben Silver, who lead the study, said: “Despite decreases in pollutant concentrations during the last ten years, China continues to suffer from poor air quality and a large disease burden resulting from air pollution.
“Our study provides insight into the effects of future emission reductions and can help inform development of effective air pollution mitigation strategies.”
Life support technology for lower income countries

For people severely ill with covid-19, the key intervention is to help them breathe. To keep them alive long enough for their own immune system to defeat the virus.
In well-resourced health care systems, there has been a rush to increase the number of hospital ventilators.
That’s not an option in low to middle income countries where they don’t have the ability to buy new equipment and where hospital oxygen systems are more basic.
But in the School of Mechanical Engineering, Professor Nikil Kapur and Dr Pete Culmer have developed an alternative solution, one that uses conventional medical equipment and a re-designed Venturi valve.
Venturi valves are small devices which are used to increase the flow of oxygen to patients.
The Leeds team have re-modelled the valve. The LeVe or Leeds Venturi valve conserves hospital oxygen supplies while delivering a mix of oxygen and air to patients in a form known as CPAP or continuous positive airway pressure. Studies from China have shown that CPAP is an effective therapy for covid-19 patients.
The LeVe can be made simply on a 3D printer, or cheaply manufactured in a workshop. In low to middle income countries, health care systems do not have access to high pressure oxygen.
The LeVe system is designed to be modular; multiple patients can receive CPAP from a single compressed air supply, combined with a single LeVe valve per patient.
Dr Pete Culmer said: "The valve is robust and easily manufactured with the intention of being used in countries where health resources are very stretched. It allows hospitals and clinics to adapt their existing equipment to increase the number of patients who can receive oxygen."
The valve is robust and easily manufactured with the intention of being used in countries where health resources are very stretched.
The team are working with the Medical Aid International charity to get the system trialed in a low to middle income country. The research has been funded by the UK’s Global Challenges Research Fund, administered by UK Research and Innovation.
Keeping science on message

Design seems to be a world away from the reality of covid-19 research. But nothing could be further from the truth.
In operating theatres, surgical teams are wearing more PPE. That makes it harder for them to fill out a pen-and-paper surgical checklist. Introduced in the NHS more than 10 years ago, the checklists are mandatory for surgical teams as they reduce the risk of mistakes.
Under the leadership of Professor Maria Lonsdale, the deputy head of the School of Design, researchers have developed a computer-based checklist that can be accessed from a phone. Surgeons no longer need to write anything: instead, they respond by clicking boxes with a finger and making voice recordings.
The work was done as part of a COVID-19 challenge run by the National Institute of Health Research MedTech Co-operative, based in Leeds. That identified the problems staff had in working in PPE.
David Jayne, Professor of Surgery, said: "There is no doubt that working in full PPE creates an additional challenge for the surgical team but the ingenuity of colleagues across the University, in this case the School of Design, is enabling us to adapt to a new way of working."
Working in full PPE creates an additional challenge for the surgical team but the ingenuity of colleagues across the University, in this case the School of Design, is enabling us to adapt to a new way of working.
The School of Design has also helped nurses at Leeds Teaching Hospitals NHS Trust produce a pamphlet and video explaining to patients and carers how to treat venous leg ulcers at home. The ulcers take a long time to heal, can be painful and are prone to infection. Many people with venous leg ulcers are cared for by community nurses. But as the NHS re-organised to deal with the peak of the covid-19 pandemic, home visits declined.
For Professor Lonsdale, the work has demonstrated the critical role that designers play in making sure information is clear, concise - and on target.
“Information design is both an art and a science. It is about the way we ensure a message connects with the right audience and is understood in the way intended.
Professor Maria Lonsdale said: "We apply a user-centred design process to the way information is communicated. We develop prototypes and test them - was the message communicated effectively, in the way that was intended and was it inclusive – and we reiterate that process until we get it right. And in healthcare, where instructions have to be unambiguous, there is a need for effective information design."
We develop prototypes and test them - was the message communicated effectively, in the way that was intended and was it inclusive – and we reiterate that process until we get it right. And in healthcare, where instructions have to be unambiguous, there is a need for effective information design.
Outsmarting the deadly shapeshifter
The Astbury Centre for Structural Molecular Biology is part of an international collaboration using computer simulation to discover new anti-viral drugs to treat COVID-19.
Their focus is the viral helicase, a protein involved in replicating the viruses’ genetic material. Through simulation created on high-performance computers, scientists can try and see how drugs could potentially disrupt this process.
The simulations at Leeds are being run by Dr Sarah Harris, an Associate Professor in the School of Physics and Astronomy.
Dr Sarah Harris said: "Drug-design is so challenging because the proteins we are trying to target are always changing shape. High-performance computing is the only way we can visualise these motions in atomic detail. Our models show us how this motion affects interactions with potential drugs, so speeding up the time it takes to develop effective therapies."
Drug-design is so challenging because the proteins we are trying to target are always changing shape. High-performance computing is the only way we can visualise these motions in atomic detail.
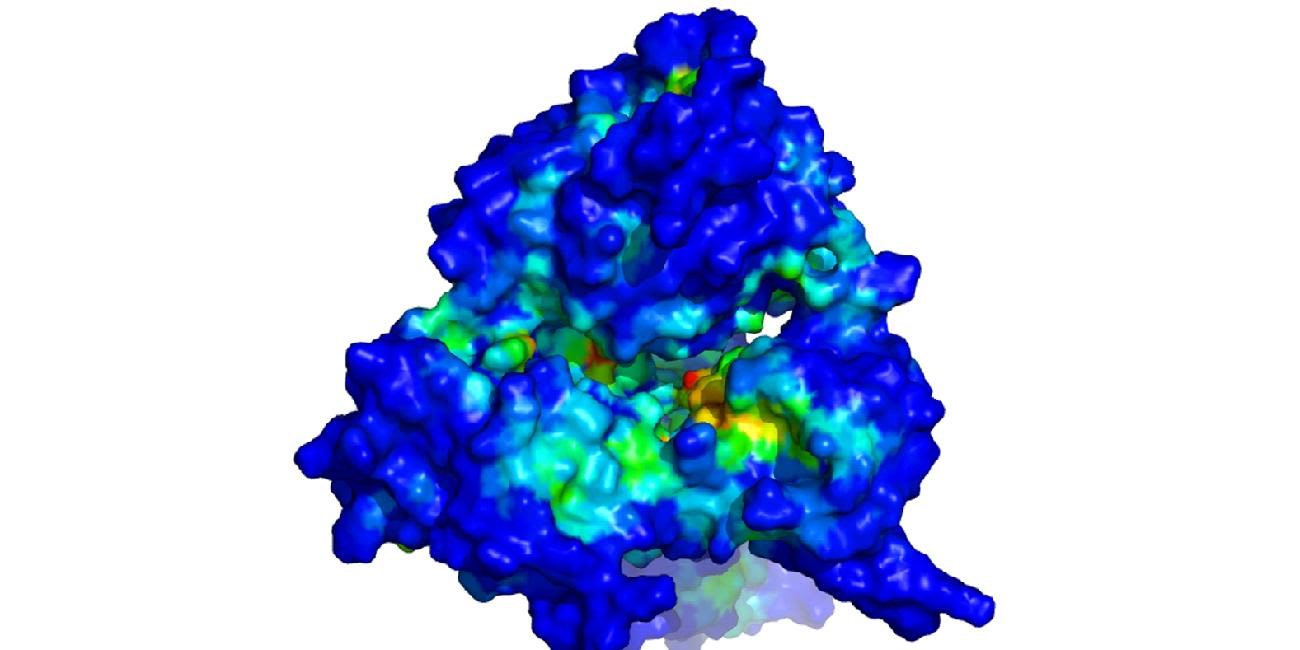
A computer simulation of the helicase in the coronavirus that causes COVID-19. Understanding the shape of the virus will help scientists design drugs to tackle it.
A computer simulation of the helicase in the coronavirus that causes COVID-19. Understanding the shape of the virus will help scientists design drugs to tackle it.
The collaboration involves scientists working in structural biology, medicinal and computational chemistry and theoretical physics, and includes researchers from UK, Germany, France, Italy and the USA.
The work is happening under the umbrella of the CCPBioSim and HECBioSim projects, which are supported by the Engineering and Physical Sciences Research Council.
Rapid, high-quality drug trials

Professor Julia Brown, Director of the Leeds Institute for Clinical Trials Research and the UKCRC Registered Clinical Trials Unit Network, is involved in a drive to fast-track clinical research into new diagnostic tests, treatments and vaccines for COVID-19.
Professor Julia Brown said: "Clinical trials are central to understanding that an intervention is truly effective. Without them, we will be unable to determine what works and for whom. By bringing a panel of experts together to prioritise the best research, we can enable clinical trials research to happen at pace ensuring that a rigorous evidence base is built as quickly as possible."
Clinical trials are central to understanding that an intervention is truly effective. Without them, we will be unable to determine what works and for whom.
Professor Brown sits on the Urgent Public Health COVID-19 Research Group, coordinated by the National Institute for Health Research.
The aim of the group is to review proposals for research into COVID-19 to ensure that the most critical can be prioritised and supported. Professor Brown is co-lead of the panel of experts which provides the group with advice on clinical trial methodology and statistics.
Professor Brown added: “Evidence-based medicine is desperately needed to tackle the covid crisis."

Professor Julia Brown
Professor Julia Brown
Out of over 500 applications, the group has so far given approval to 49 trials, including Oxford University’s investigation into a vaccine for COVID-19 and a study by Cambridge University and Kings College, London, into whether re-purposed drugs can be effective in reducing the severity of the disease. More studies are in the final stages of review.
A quick, reliable test for COVID-19 antibodies
Research into antimicrobial resistance is to be adapted to see if it can be used to develop a quick and reliable test for COVID-19 antibodies.
Professors Christoph Walti and Lars Jeuken and their teams in the School of Electronic and Electrical Engineering and Faculty of Biological Sciences have developed a prototype biosensor assay to help doctors diagnose whether a patient is suffering from a bacterial infection and can be treated with antibiotics - or a viral infection, where antibiotics would be ineffective.
Professor Christoph Walti said: "I think we can adapt the technology we are developing to stop the overuse of antibiotics. We are investigating the use of protein switches that would indicate the presence of COVID-19 antibodies. The aim is the develop a disposable test that can determine in under a minute whether someone has been infected with the virus."
The aim is the develop a disposable test that can determine in under a minute whether someone has been infected with the virus
At the heart of the device is a synthetic “protein switch”. If it registers the presence of biomarkers indicating a bacterial infection from a small blood sample, it generates an electric signal which is picked up by the device.
Professor Walti believes protein switches can be used to identify whether someone has antibodies to COVID-19, indicating whether they have had the infection.

Professor Christoph Walti
Professor Christoph Walti
The researchers are collaborating with immunology researchers being led by Professor Francesco Del Galdo.
Attempts by other research organisations to develop mass screening for COVID-19 antibodies have run into technical difficulties.
Using robotics to reduce the COVID-19 threat

The University STORM lab is refocusing its work to see if it can find a solution to the problem that has brought all but emergency and essential flexible endoscopies to a halt.
Pietro Valdastri, Professor of Robotics and Autonomous Systems, University of Leeds, said: "In 2017, there were more than 2 million flexible endoscopies carried out in the UK – and they play an important part in cancer screening. There is an urgent need to find a way of developing an endoscopic system that is safe for patients and staff – and the research at Leeds puts us in a very strong position to do that."
There is an urgent need to find a way of developing an endoscopic system that is safe for patients and staff – and the research at Leeds puts us in a very strong position to do that.
Flexible endoscopy is a medical procedure that enables doctors or other healthcare specialists to pass a tube into the gastrointestinal tract to examine the oesophagus and stomach, or into the colon and bowel.
From April, all routine flexile endoscopies have stopped because of the risks they pose to healthcare staff administering the procedure. Carrying out the procedure creates an aerosol of body fluids that could transmit the coronavirus. Also, there is no evidence that the current process for cleaning endoscopes between patients destroys the coronavirus.
For more than 10 years, Professor Pietro Valdastri, who leads the STORM lab, has been developing low-cost, semi-disposable endoscopes for the upper gastrointestinal tract, and a semi-autonomous robotic system that guides a very small medical device into the bowel and colon to take images and biopsies.
The challenge facing Professor Valdastri and his team is to bring those technologies together, to develop a system that would allow the medical team to be separated from the patient, which is possible if a robot is controlling the device, and for sections of the endoscope equipment to be used once and then safely disposed of.
His belief is the robotic system, which uses magnets to guide a small capsule through the gastrointestinal tract, could be adapted to perform flexible endoscopies with a reduced risk of COVID-19 transmission.
Further Information
Read more about how University of Leeds expertise is leading the way on coronavirus-related research – including the recovery.
Find out how the University's senior researchers are advising the Government on the complex issues surrounding coronavirus and lockdown, including advising SAGE - the Scientific Advisory Group for Emergencies.