Medicine Matters
The impact of the COVID-19 pandemic on our students

Innovating for the future


Vaccine for the heart and mind
- the reimagined Thackray Museum of Medicine
When the Thackray Museum of Medicine closed its doors in May 2019 to begin a top to tail refurbishment, no one imagined that it would be two years before its elegant Victorian front door could be thrown open once more to the public.
In the intervening period, not only has the museum seen a transformation of its building and galleries but it has also found itself at the heart of the pandemic. Overnight, the boundary between the history in display cases and history in the making became very permeable indeed. The museum was the first anywhere to host a vaccination centre (for the Pfizer / BioNTech vaccine) and has also been a centre for vaccine trial clinics. A new commitment to contemporary collecting was put quickly into action as the museum worked with others to develop and implement a COVID-19 collecting programme.
There has perhaps never been a time when medical museums have been so relevant. The reimagined museum traces the story of modern medicine through the stories of people – from the overcrowded slums of industrial Leeds to the cutting edge of new healthtech.
These stories are designed not only to inspire people to discover their own part to play in helping to build a healthier society but in many cases they have been co-curated and co-created with communities around the region. To create the displays, the museum’s team was complemented by 200 collaborators – from artists, academics and clinical practitioners to members of community groups. The result is a museum that really does have something for everyone.
Eleven brand new galleries have been created and the museum’s much-loved Victorian Street has also been given a makeover. The result is an immersive and compelling story of medicine that takes the visitor on a journey from people’s daily struggles against disease, through the origins of modern surgery, germ theory and public health to the most influential technological breakthroughs of the last two centuries. The significance of crisis as a driver of human ingenuity and innovation is graphically drawn out in a gallery that focuses on our collective response to war and pandemics.
The wider medical, social and political implications of what society deems a ‘normal’ healthy body and mind are critically and entertainingly challenged through a series of co-curated displays from diverse perspectives. The emotional and individual context of surgery is beautifully told through a contemporary artist’s film inspired by the UK’s first double hand transplant. The scale of human endeavour represented by medicine is captured in a gallery that celebrates the multitude of people involved in healthcare – from hospital nurses to the keepers of family remedies. The galleries are designed around spaces where people cam take the time to explore topics further – a tinkering space for hands on inventing; a debating space for delving deeper into ideas and breakout spaces to read and reflect – or just to relax and let the phenomenal scope and richness of the museum’s stories sink in.
The new displays provide an immersive and interactive setting for the museum’s unmatched collection of medical technologies and supplies – from iron lungs to Prince Albert’s personal medicine chest. The Wilkinson Collection of apothecary jars has been reinterpreted and represented in an apothecary shop display that beautifully evokes the roots of pharmacology. The 3,000 or so fascinating objects on display are complemented by a new online database featuring 50,000 objects from the museum’s collection. Along with a whole new suite of activities, events and digital learning resources, the museum has been designed to be a space that will offer every visitor and every visit a new encounter and new discoveries, no matter how often they come back for more.
The museum’s normal (non-lockdown) hours of opening are 10am – 5pm, Monday - Sunday.


Finding new ways to communicate in a crisis
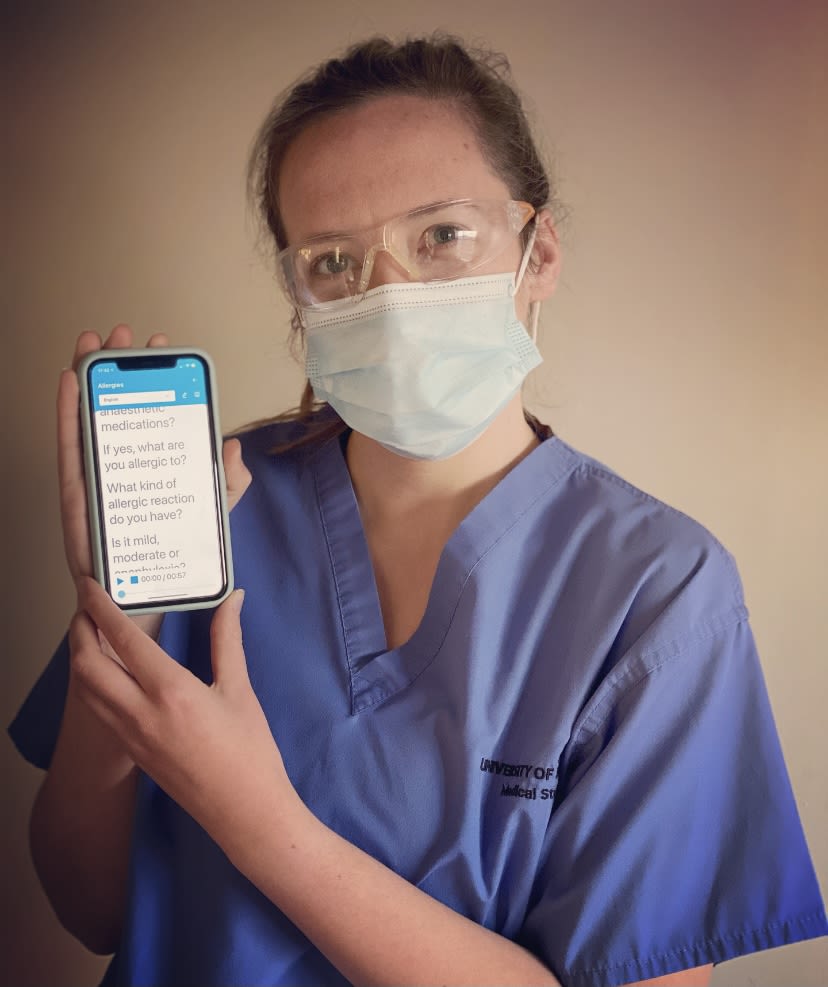
Scarlett Brandley, MBChB Year 5
Scarlett Brandley, MBChB Year 5
Due to the COVID-19 pandemic, I had the task of finding a new elective in the United Kingdom that was appropriate to undertake amidst a pandemic. Having worked as a Healthcare Assistant in paediatric theatres prior to medical school, I contacted Dr Rachael Grimaldi, an anaesthetic registrar, who had developed CardMedic, a novel disaster innovation response to COVID-19.
CardMedic is a digital communication resource, comprised of an extensive list of topics related to patient care and manag ver-growing list of topics, CardMedic has already shown to be of great benefit as an aid to better patient communication and care. It’s available in multiple languages, with a read-aloud option available for patients who are partially sighted or blind, a free-text section for direct communication, and soon to be uploaded accessible versions of the flashcards for patients with underlying communication difficulties, with simple English, images and symbols, created by a team of Speech and Language therapists (SLTs) and Learning Disability (LD) nurses.
I’m fortunate to continue working with Dr Grimaldi on CardMedic, writing new content and continuing to assist the SLTs and LD nurses. I’m extremely fortunate to have found an elective that has provided me with the chance to network, the chance to develop my skillset and the chance to further my understanding of the health inequalities that COVID-19 has intensified.
Stepping up in a pandemic


Professor Paul Stewart, Advisor on Health Policy & Research
Professor Paul Stewart, Advisor on Health Policy & Research
Exploring the impact of the COVID-19 pandemic
In February the Faculty organised a joint webinar with the University’s Alumni and Development team to explore the impact and realities of the COVID-19 pandemic.
The popular online event, attended by over 240 guests, recognised some of the extraordinary and ongoing efforts of the University community during the pandemic.
Professor Paul Stewart, Advisor on Health Policy & Research spoke about the impact of COVID-19 on the Faculty’s 1,200 staff and 5,000 students, as well as the changes that have been implemented to enable the continuation of research and teaching in Medicine, Dentistry, Healthcare and Psychology.
Attendees also heard from Dr Manoj Sivan, Associate Clinical Professor in Rehabilitation Medicine, who discussed his research into the scale of the long term symptoms of COVID-19 and the need for timely and targeted rehabilitation interventions.
As part of the webinar, two current Leeds students shared their experience of how University life has changed as well as the realities of undertaking placements in these exceptional times.
Final year medical student Chantelle Waddington was one of those that spoke: “It’s been really rewarding to have been able to make a difference. I’m amazed by all of our NHS colleagues and have been so impressed by how accommodating staff on placement have been in helping us develop our experience.”
Feedback from the event was overwhelmingly positive with one attendee saying: “The webinar gave me a real insight to the lives and bravery of so many. Thank you for the opportunity to learn of the dedication of those of whom have and will continue to follow their calling.”
Watch the replay of the event below:
Students support testing and vaccination efforts in Leeds
Over 200 students from the Faculty of Medicine and Health have been trained to work in the University’s asymptomatic testing centres on campus. The University set up testing centres in the Refectory and The Edge to offer free and fast asymptomatic coronavirus tests on campus, initially for students who wanted to leave their university accommodation for the winter break. The centres have remained in use for asymptomatic testing for staff and students who need to be on campus to deliver essential services or to support students in certain subjects, such as medicine and dentistry, to continue their studies uninterrupted.
In addition, students have also been trained to administer the COVID- 19 vaccine at centres across Leeds which have been available to the public.
Two medical students outline why they got involved to work at the centres.
“I chose to work at the testing centre because I thought it was a good opportunity to get involved and do my bit during the pandemic. It was a great way to help the university out as I had some extra time during my placement when I applied. As a year 4 medical student, it’s really beneficial to know what going on in both the education and healthcare sectors and to see the difference in the implementation of measures to help with the pandemic.
It’s been really lovely being able to see people feel more confident about getting back to some form of normality and provides reassurance to people that they aren’t passing on the virus to their loved ones. It has also given me the chance to meet some younger year students in various healthcare areas and the impact it has had on their university experience has been pretty detrimental. This was a good way of helping to be safe, particularly when travelling home to family and give them some hope of a path to some form of normality.”
Daneille Murdock, MBChB Year 4
“During the first lockdown I wished that I was more qualified so I could do more to help. When it came to November and I saw an advert through Leeds University Union for a job on the vaccine programme, I knew I had to go for it. A couple of months later and there I am, standing in the Elland Road COVID-19 Mass Vaccination Centre, waiting for my first patient to arrive.
I felt a mixture of excitement to be finally starting the role, nervousness about vaccinating my first person and pride that I was doing something to give back. Having helped deliver flu vaccines before on my GP rotation this year, I wasn’t nervous about giving the injection itself, more how people would react, given the negative press surrounding public perceptions of the vaccine. What I didn’t expect was the immense gratitude that my colleagues and I would receive from the public. Every person was incredibly thankful and took the time to praise us all for our work in vaccinating the population.
What I really love about the job is that I feel like my efforts are really making a difference. Being part of a team helping to vaccinate several thousand people every day is really rewarding. It reminds me of the reasons why I applied to medicine in the first place – to work with the public and to save lives. Every time I go to work, I become more and more excited to finally qualify as a doctor.”
Alex Flach, MBChB Year 4

Students at the University's COVID-19 testing centre
Students at the University's COVID-19 testing centre
Leeds Paralympian on the NHS frontline

Kim Daybell
Kim Daybell
For many athletes, the postponement of the Tokyo 2020 Paralympics meant putting their dreams of sporting success on hold.
But for Dr Kim Daybell (Medicine 2018) it meant a return to helping those who needed him most. Kim, a junior doctor in the Whittington Hospital, North London, has treated COVID-19 patients throughout the pandemic.
A two-time Paralympian and a member of Team GB’s Paralympic table tennis squad, Kim was due to compete in Tokyo last summer. But instead of stepping up his training for the Games, he stepped onto the NHS frontline.
“I was working part time as a junior doctor, part time table tennis,” says Kim. “The plan was to finish my Foundation Year and then start with table tennis full time in preparation for Tokyo. That’s when COVID-19 hit, the Paralympics were postponed, and they asked if I’d come on the full-time rota, which I did.”
For many athletes – Kim included – the postponement had serious implications. “Obviously people might say ‘well they just have to wait a year’. But a year is a long time in sport, especially in the Paralympics where athletes have deteriorating conditions.
“I was lucky to be in a position to fight back. I wanted to help as much as I could – we join the health service for these exact situations.”
Engaging with Climate Change


Solving the climate crisis through creativity
In early 2018, a group of organisations and companies from the cultural and creative sectors of Leeds came together to respond to the climate crisis. From this, Sustainable Arts in Leeds (SAIL) was formed to share and establish best practice to reduce the carbon footprint of the creative sector. But through collective influence to engage everyone in climate change awareness, it doesn’t stop there. Jamie Saye, Founder of SAIL, talks to student reporter Grace Rahmatallah.
Can you tell me about the work of SAIL?
We’re a community interest company and our aim is to unite the creative and cultural industries of Leeds so that we can tackle climate change at the local level. We learn from each other and we share best practice training as well. We’ve negotiated ways to get the organisations within SAIL to have lower carbon footprint through having a renewable energy tariff which we’ve secured, and then we’re also using our power as a network to lobby for changes at a council level, to support organisations to become more sustainable as well. We recently hit the 100-member mark so as a sector it seems like we are starting to move in the right direction.
What have you learned through your work with SAIL which could be transferred to improving medical education?
Developing understanding of what the science behind climate change is and how we got to this point and how this affects people’s health, the obvious stuff around air pollution. For example, fossil fuel polluting vehicles and industries spewing out all this stuff which we’re then breathing in, their potential impacts on our food supply and potential increased amounts of stress due to things like transport breaking down because of floods. It’s interconnected, and climate change doesn’t exist in this vacuum. It’s pervasive in literally everything and there’s no point in ignoring it.
What would you advise to doctors and other health care workers to improve sustainability?
There’s so many things you can do that aren’t particularly sexy but really work and that’s why I think a lot of things get ignored. There are simple things like looking at what energy your workplace is using and why it’s using it, and not assuming that it’s someone else’s job to think about that, because everyone else may think it’s everyone else’s job. Just think about what you’re doing and why you’re doing it. Continuing to do something because that’s the way it’s always been done is the worst reason to ever do anything ever. Evaluate your processes. Look at your buildings. Look at the obvious stuff, or maybe not so obvious stuff or look at the boring stuff, because that might be where you can make the biggest gains. Like procurement, often you just get the thing that’s easiest or cheapest, and that’s usually not the best for sustainability.
What advice can you give to somebody who wants to promote attitudinal change in light of sustainability?
I think if you can explain why these attitudinal habits are so important then that conversation becomes easier to have. Also, making people understand what is within their sphere of influence, because I think especially for climate change, it can feel like this monstrous all-encompassing thing that you’re like, “how on earth as an individual can I have any sort of impact on that?”. And you can, there’s so much you can do. I think it’s recognising what is within your control, that is quite important. And then once you kind of solve the thing that’s within your control, then you can go “OK, what’s the next thing?” And then work from there, but it is hard that kind of initial change. It’s addictive, it starts with recycling and then you end up starting your own company!
Interview by Grace Rahmatallah,
BSc in Applied Health (Medical Education)

Monty Losowsky Memorial Lecture

Monty to be remembered in opportunity for students
Professor Monty Losowsky was not only a past Dean of the Medical School and Professor of Medicine, he was also the much admired President of the Thackray Museum of Medicine, housed in the old Workhouse at St. James’s University Hospital.
This year, to honour his memory, a joint collaboration between the Leeds Medical School and the Museum will see the inaugural Annual Monty Losowsky Memorial Lecture which will be a competition open to all students at the School with a first prize of £1,000, kindly sponsored by Leeds based OneMedical Group, a medal and a place on an Honours Board within the Faculty.
Leeds alumnus, Dr Neil Kaiper-Holmes, the current Chair of the Museum, said: “We are very pleased to mark the tremendous contribution that Monty made to medicine in our city with this competition which we hope will be a fitting tribute in recognising the lifetime interest that Monty had in medical education. Students will be encouraged to write a lecture on any medical topic, past, present or future and the best three will then give their lecture to a live audience in front of an eminent judging panel with the winner recognised in perpetuity in their Alma Mater as well as with a welcome boost to their finances.”
This year the final will be held on Thursday 14 October as a virtual event, but it is anticipated that in future years it will be held in a suitably prestigious venue such as The Great Hall of the University, the Museum or the Town Hall in Leeds.
Recommended reads

Poverty Safari
By Darren McGarvey
Review by Serena Waters, Intercalated BSc International Health
Darren McGarvey takes us on an angry, powerful and incredibly personal journey through experiences growing up in poverty, in Pollok - one of the most deprived areas of Glasgow. In this book, we learn about how trauma, exposure to violence and ultimately stress, can shape someone’s entire life, and play a role in future addiction and mental health.
McGarvey argues that poverty is misunderstood from across the political spectrum, and often interventions by local governments fail to acknowledge what people living in deprived areas actually want and need.
McGarvey does well to challenge our assumptions and shows insight into how his stereotyped views about the middle classes have been wrong in the past. He urges us not to be swept up by tribalism and cancel culture, and to open a dialogue with those who have a different view to you.
Overall, Poverty Safari is a nuanced, unfiltered and shocking account of how working-class people can feel alienated by society and failed by political systems. I think that it will enable me to become a more compassionate doctor in the future, as it opened my eyes to the realities of addiction and the incredible personal strength that it takes to overcome this.
Invisible Women: Exposing Data Bias in a World Designed for Men
By Carlo Criado Perez
Review by May Schymczyk, MBChB (Year 2)
An essential read for any budding clinician, this book explores how the gender data gap inconveniences, discriminates and leads to increased morbidity and mortality in 50% of the global population. Perez, the feminist campaigner whose opposition to removing women from banknotes earned her an OBE, turns her steely gaze to topics ranging from the economic underappreciation of unpaid female labour to phones being unsuitably sized for a woman’s hand.
Her damning analysis of medical research however is perhaps the most revealing aspect of the book. The gross underrepresentation of women in clinical trials, particularly those who are pregnant or from an ethnic minority background, is seamlessly linked to adverse outcomes. In addition, Perez highlights how medical education conditions student doctors to think of the male body as the default human body. From textbooks to consultations, this bias results in the misdiagnosis of common conditions, harmful prescriptions and cultural misunderstanding of how women express and feel chronic pain.
Throughout, Perez’s arguments are not only meticulously researched and referenced, but are recounted with wit, warmth and humour. It’s a refreshing perspective that can help contextualise the lived experience of female patients and our own, within healthcare systems and beyond. By the last page, you are equal parts enraged, entertained and determined to make a positive change.
x minus y

You live in London on the moon,
250,000 miles and months away,
down South.
You call me when you fall and plunge
in lunar seas of crises, clouds
or craters fathoms deep.
I offer light in seconds, hours, over years,
hope it finds your shadowed self,
half-hidden from the sun.
You ask me, sometimes,
if my sky is overcast or filled with meteors and stars.
I don’t know what to say.
My Northern nights are unpolluted, clear and bright
I search for constellations
I can’t name in empty dark.
I study orbits, phases on a calendar,
the apogee and perigee
that rule our interaction.
Then put on walking boots, a mask and plot
eccentric paths across the universe to you.
Poem written by:
Dr Emma Storr, Visiting Associate Professor
Keeping in touch
You can find us @LeedsMedHealth where we share news, views and details of events.
Contact us at medicinecomms@leeds.ac.uk.

Editoral Board
Editor
Professor Trudie Roberts
Professor of Medical Education
Deputy Editor
Gillian Neild
Faculty Head of Communications
Professor Peter Howdle
Emeritus Professor of Clinical Medicine
Mr Mark Dorey
Senior Communications Manager,
Alumni and Development Team
Professor Laura Stroud
Deputy Dean, School of Medicine
Dr Emma Storr
Medical Humanities Lead and Primary Care
Alison Ledger
Head of Intercalated Programmes
Vicki Harper
Clerical Assistant
Student representatives:
Bethany Chandler
Alexander Flach
Medicine Matters is produced biannually by
the Leeds School of Medicine.