Three ways Leeds has contributed to the global fight against cancer

Today (5 July 2023) marks 75 years of the National Health Service. Treating more than a million people a day in England alone, the NHS ensures treatment isn’t just a privilege for those who can afford it – and that everyone has access to life-saving care.
To celebrate, we’re taking a look at some of the ways scientists at the University of Leeds have directly contributed to the way cancer is treated on the NHS.
Pioneering radiotherapy, a cornerstone of cancer treatment

Today, if you receive radiotherapy at Leeds Cancer Centre, your treatment can now be determined using the new MRI simulator – a state-of-the-art machine that can precisely determine the targeting of radiotherapy that uses shaped beams of high-energy radiation, minimising damage to surrounding tissues.
“Radiotherapy has evolved dramatically since the early days of the NHS,” says Professor David Sebag-Montefiore, Academic Clinical Oncologist at the University of Leeds.

Professor David Sebag-Montefiore, Academic Clinical Oncologist at the University of Leeds
Professor David Sebag-Montefiore, Academic Clinical Oncologist at the University of Leeds
Thanks to decades of research, today’s radiotherapy is highly sophisticated, highly targeted, and suitable for pretty much everyone who needs it.
Leeds scientists have played major roles in the development of radiotherapy. While working in Australia in the early 1900s, Leeds physicist William Bragg made an important discovery about how radiation loses energy, which later became crucial in designing treatment strategies for radiotherapy. Bragg and his son Lawrence were later awarded the Nobel Prize in Physics for their discovery of X-ray crystallography during their time at Leeds. Today this method is invaluable in allowing scientists to study the molecular mechanisms involved in cancer and how new drugs might be developed to stop it.
Later, in 1929, Leeds led a major fundraising campaign to buy large amounts of radium, and in the 1930s, Leeds General Infirmary became the national radium centre, treating around 1000 patients with radium each year.
But at the time, radium was a locally applied treatment and so only suitable for some types of cancer within easy reach. Leeds researchers have since made radiotherapy widely applicable to a range of cancers, by exploring different sources of radiation and delivery techniques to reach tumours deep within the body with less impact on healthy tissues. And through clinical trials, our scientists have established how it should be used in combination with other therapies, like surgery and chemotherapy, for a range of disease types and stages. “It’s incredibly rewarding when your research changes clinical practice, and improves outcomes including quality of life for patients,” reflects Professor Sebag-Montefiore.
We’re also leading trials that suggest radiotherapy can be just as effective at treating some types of cancer as surgery, which takes longer to recover from and can cause life-long side effects. For rectal cancer, for example, this could mean curing patients without the need for major surgery or a colostomy bag. And for early-stage lung cancer, a short, out-patient course of targeted radiotherapy can provide a much-needed alternative to invasive surgery. Since cancer disproportionately impacts people from lower socio-economic backgrounds – who may also be less likely or able to have surgery due to other factors and health conditions – this work is contributing to a nationwide effort to tackle inequalities in healthcare.
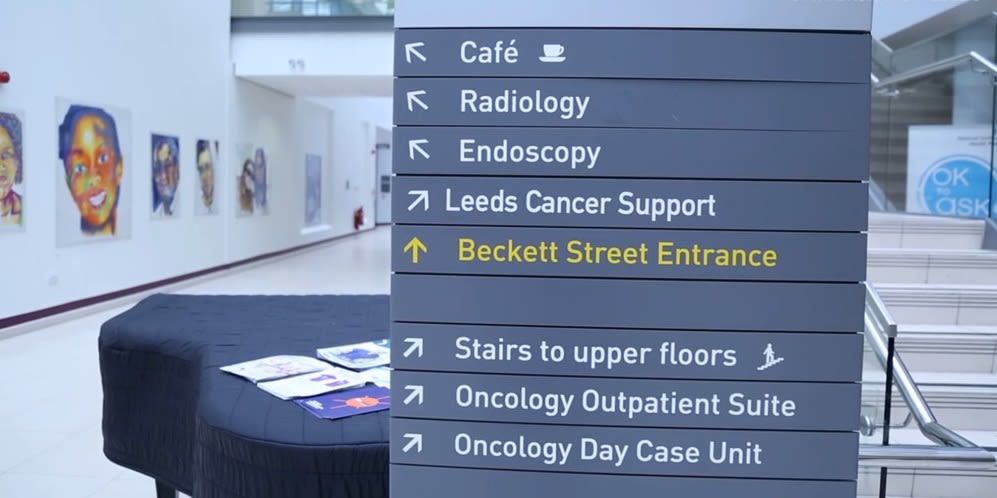
Leeds Cancer Centre in the Bexley Wing of St. James's University Hospital (image: University of Leeds)
Leeds Cancer Centre in the Bexley Wing of St. James's University Hospital (image: University of Leeds)
Leeds Cancer Centre today serves 2.8 million people from Leeds and the surrounding area, and in 2019 was awarded £3.5m to establish a Centre of Excellence for Radiotherapy Research, with Professor Sebag-Montefiore at the helm. “Our vision is to turn radiotherapy into an even more targeted treatment, using tools like artificial intelligence and treatments like immunotherapy,” he says.
I’m hopeful that in the future – perhaps before the NHS’s 100th anniversary – we’ll be able to cure most people’s cancer with personalised radiotherapy, as an out-patient, in as little as one week.
The birth of tamoxifen and a new era of chemoprevention

Bringing a drug to patients can be a long and winding road. “Science meanders,” says Dr Kersten Hall, scientific historian and visiting fellow at the University of Leeds. “It goes round corners, up blind alleys, seeks collaboration – and it’s all the more interesting for it.”

Dr Kersten Hall, scientific historian and visiting fellow at the University of Leeds
Dr Kersten Hall, scientific historian and visiting fellow at the University of Leeds
This is certainly the case for tamoxifen, a drug which blocks cancer cells from interacting with the hormone oestrogen. Today, it’s hailed as one of the most important drugs in medical oncology and is used around the world to help some people reduce their risk of breast cancer by more than 50%.
But without the perseverance of Leeds and Cheshire scientists across the 1960s and 70s, tamoxifen – then named ICI-46474 – may have been shelved as a failed contraceptive. “Scientists were trying to make an emergency morning-after pill,” explains Dr Hall. “But when testing this compound in people, it actually increased ovulation – the opposite of what you want in that scenario.”
Dr Arthur Walpole realised ICI-46474’s anti-cancer potential and, despite significant opposition, pushed for its development; in 1972, renamed tamoxifen, it was approved for treating late-stage breast cancer.
Tamoxifen may have stayed in the world of palliative care, were it not for Professor Craig Jordan, who studied both his undergraduate and PhD in Leeds and, after a brief stint in the US, returned to set up his research group, the ‘Tamoxifen Team’.
“In 1972, no one really cared about tamoxifen. People were told not to spend too much time investigating it, as it was not expected to succeed,” Professor Jordan describes.
The Tamoxifen Team was the catalyst that changed the way people thought about the drug.
Thanks to the team’s discoveries, tamoxifen is now prescribed on the NHS to shrink early-stage breast cancers, control breast cancer that’s spread, and prevent the disease in high-risk individuals. But perhaps most importantly, they sparked a new era in cancer research, with tamoxifen as the world’s first chemo-preventative drug. Later, Professor Jordan would build on this work to discover a new group of hormone therapies called Selective Estrogen Receptor Modulators (SERMs).
“My life’s work researching tamoxifen led me to discover SERMs, now available worldwide to treat multiple diseases in women with a single tablet,” says Professor Jordan, who was awarded an OBE in 2002 for services to international breast cancer research.
Without my education at Leeds, we wouldn’t have these advances – which have saved the lives of millions and improved the lives of untold numbers around the world.
Changing lives at the University of Leeds Clinical Trials Research Unit

Since its beginnings 31 years ago, the University of Leeds Clinical Trials Research Unit has been at the forefront of cancer research.
The centre, which specialises in the design, conduct and analysis of phase I to phase IV national and international clinical trials, is an international leader in the field and among the largest in the UK, influencing national and international clinical practice.
It was founded in 1992 as a small research group led by Professor Julia Brown at the NHS Cookridge Hospital. Joining the University of Leeds 10 years later gave the group the opportunity to expand to a research unit. By 2013 it had become a research institute, which today comprises four divisions with more than 200 employees.

Professor Julia Brown, who led the research group that later became the Clinical Trials Research Unit at Leeds
Professor Julia Brown, who led the research group that later became the Clinical Trials Research Unit at Leeds
In 2018 it was given the opportunity to expand its work even further thanks to a new collaboration with Cancer Research UK. The charity announced funding for eight specialist clinical trials units, one of which would be at the University.
Awarding almost £2m in research funding for five years, Cancer Research UK created the CRUK Leeds Clinical Trials Unit, with a focus on researching and testing better and kinder treatments for patients.
Based at the University of Leeds Institute of Clinical Trials Research, the unit focuses on patients who are treated with radiotherapy or have blood or colorectal cancers, giving them more access to innovative treatments by significantly increasing the number of clinical trials led by Leeds.
The success of the unit has led to a further £2.9 million in infrastructure funding being allocated in 2023, meaning its vital work will continue for a further five years.
Over the decades, research carried out by scientists at the Leeds Clinical Trials Unit has led to changes in the way a range of cancers are treated around the world.
Research in the unit's myeloma portfolio has led to changes in standard of care. In 2003 our research (Myeloma VII) showed treatment with a stem cell transplant was beneficial for patients with newly diagnosed myeloma, while in 2021 data from one of its trials (Myeloma XI) was used to support patients receiving maintenance treatment with a chemotherapy drug called lenalidomide after transplant. This highly effective treatment combination is now used globally. Furthermore, patients with relapsed myeloma can receive a second transplant based on results of its Myeloma X trial (2013). All these treatment advances have been shown to improve life expectancy.
The Leeds Clinical Trials Unit MRC CLASICC trial which was set-up in 1996 showed keyhole surgery was a suitable option for colorectal cancer and improved recovery times after surgery. Keyhole surgery is now used globally to treat colon and rectal cancer.
And research into oesophageal cancer for older patients (GO-2 – 2018) showed they could safely receive lower doses of chemotherapy, leading to fewer side effects and the same cancer outcomes. This has been accepted as standard of care by the NHS, improving outcomes for more frail patients who may not have been able to tolerate higher doses of chemotherapy.
Looking forward, the Leeds Clinical Trials Unit will continue to focus on radiotherapy and cancers of the blood, as well as bowel cancer.
Professor Julia Brown, Director of the Leeds Clinical Trials Research Unit, said: “Our motivation at Leeds has always been to improve cancer survival rates. For decades, many dedicated researchers and clinicians working here have made an incredible contribution to the global fight against cancer.
“As our trials are delivered through the NHS, this means that patients across the country can benefit from new and innovative treatments, regardless of their personal circumstances. We are committed to tackling inequalities in cancer care, providing kinder, smarter treatments for cancer patients that help them live a better quality of life during and beyond their cancer journey.
“Discoveries and developments at Leeds have helped to save lives across our city, our region and indeed the world. Working alongside the NHS, we will continue in our mission to find treatments for cancer that change people’s lives.”