Learning from drills – and a dummy

As dentistry reeled from COVID-19 with practices and teaching schools closed, a group of researchers at the University of Leeds was busy investigating whether changes to dental surgery could reduce the risk of infection – and help more patients get seen after lockdown.
Unless you were suffering from severe tooth pain, going to the dentist was probably the last thing you were worrying about back in 2020.
But almost overnight, COVID-19 and the lockdowns that followed hit dentistry hard, shutting down practices and teaching schools and generating a huge backlog of patients waiting for treatment.
In fact, figures from NHS Dental Statistics for England biannual reports suggest that six million fewer adults were seen by an NHS dentist in the 24 months up to the end of 2021 than in the previous period.
All those cancelled appointments and unreported dental problems have meant the resulting treatment backlog is still being worked through today.
But a team of researchers at Leeds worked through the pandemic, seizing the chance to turn their efforts to a project with the potential not only to advance dentistry, but to help dentists treat more patients.
And, as the University’s School of Dentistry closed, like others across the UK, risking the qualification of a whole year’s cohort of new dentists, they were determined to do whatever they could.
Their findings would go on to provide tremendously informative, practical insights.
It all began with a proposal for grant funding from the British Endodontic Society, as Professor David Wood, Director of Research and Innovation at the School of Dentistry, explained.
“We had great expertise, the clinicians and the microbiologists, plus the co-operation of the local NHS Trust to actually use their facilities during that horrible period when everyone was locked out.
“But to secure the funding, we still needed to firm up the methodology in our response, which was the real challenge.
“We worked on it right up to the deadline – at midnight – with plenty of last-minute phone calls to discuss how our ideas would work in practice; an incredibly collaborative endeavour.”
A bold approach at an uncertain time

Professor Brian Nattress, Clinical Professor in Restorative Dentistry, also looks back on the project with pride.
“In my 40 years at the University, I’ve never encountered anything that had as big an impact on dentistry as COVID-19,” Brian said.
“So to feel like we were able to do something to move the clocks forward was really important.”
That ‘something’, as it happens, was a world first – a novel idea to use a harmless virus detection model which Brian, David and their colleagues were determined to deliver.
In a nutshell, the hypothesis was that by switching the drills used in dental surgery, they could reduce the spread of aerosol spray, or how particles get dispersed in the air.
The more aerosol spray being spread, the more dangerous the environment for both patients and dentists – especially at the height of a pandemic.
But to move from an idea to a funded research project would require a significant number of research hours and perseverance.
It also necessitated the involvement of the large, multidisciplinary team that had already been assembled during the proposal stage.
To feel like we were able to do something to move the clocks forward was really important.”
“I got involved as soon as the funding was granted”, Emma Black, Research Technician in Microbiology, said.
“My role was to help make it all happen from a practical perspective, which involved not only sourcing the right kit, but things like discussing the finer points of saliva flow rates and tubing requirements.
“There were lots of very technical, specific elements because it was such an innovative project.”
Dr Jon Vernon, Research Fellow, was lead researcher and author of the project’s resulting publications.
“Being unable to get into the lab at a time like that was quite nerve-wracking and alien,” he recalled.
“So when my line manager, Professor Deidre Devine, mentioned that she was involved in a study about COVID-19 and wanted me to join her, I couldn’t wait.”
There were practical hurdles to clear, though. The tests would require two products in particular – bacteriophage, or phage (a type of virus that infects bacteria) and the correct strain of bacteria to experiment on.
“As well as sourcing the consumable materials and equipment from our labs, I needed to order the bacteriophage and bacterial strain from Germany,” Emma explained.
“But this was in the middle of the pandemic, so it was difficult to get a reply.
“I was ringing them on the phone but nobody was answering – because, of course, there was no-one there in the office on the other side.”
Dr Louise Fletcher, Lecturer in Environmental Engineering, meanwhile, was asked to help from an engineering point of view thanks to her expertise in sampling bioaerosols – biological particles in the air – in indoor and outdoor environments.
“It’s great to work with microbiologists from both dentistry and engineering; just bringing all those little bits together,” she said.
“Everybody had – and has – something to contribute.”
As true to life as possible

Let’s fast-forward to the actual experiments, though – because they’re fascinating.
What sets the project apart is the fact that it used a real, although harmless, surrogate virus similar in size and structure to SARS-CoV-2, which causes COVID-19.
Never before had a harmless COVID-19-like virus been analysed during routine drilling procedures; a world first.
“That was the lightbulb moment right at the start, when we were submitting our application,” David said.
“We’d studied the literature on other uses of surrogate viruses for looking at things like the effectiveness of hand washing programmes, but for this context, the key was thinking about aerosolising that virus.”
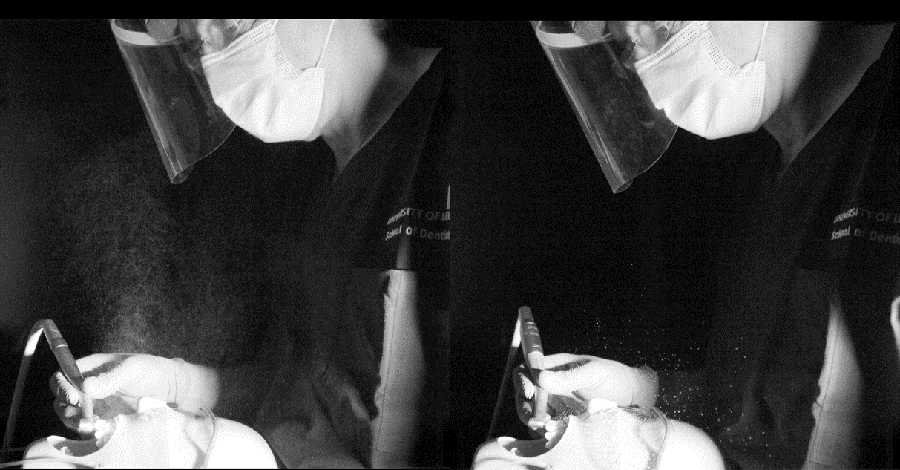
We must also mention the ingenious, if somewhat uncanny, dummy head that was used along with simulated saliva to measure the difference between the level of aerosols generated through the use of different dental tools.
The dummy head
The dummy head
Ultimately, the team found that by using more modern, lower-speed electric drills instead of conventional air-driven alternatives, the aerosol spray was virtually eliminated, creating a safer environment within the practice and reducing the time to prepare surgeries.
“In pre-testing in the lab, I had been putting the phage in a squirty aerosol bottle to spray it in a cabinet and see if I could actually aerosolise it,” Jon said.
“There were detection limits to consider. We were still trying to learn how to handle the phage, and I hadn’t really done much viral work in the past – but I was feeling confident because all the signs were pointing to it being successful.”
Yet the team knew patience would be required.
“In the first clinic, we got all 300 plates back and there was nothing on them, no viral detection,” Jon said.
Louise echoed that need for patience:
“Microbiology is always really, really difficult, because things don’t always grow when you want them to grow.
“In a three-year project, that’s not too much of an issue, but in a very short project like this it might sometimes be frustrating.
“Thankfully, we managed to bring our expertise together – and the impact was amazing.”
Indeed, when the approach shifted to look at the front teeth instead of those at the back, the results started to flow.
The project was still in its early days, though.
What followed would involve approximately 120 hours in the clinic, around 3,500 agar plates and a massive team effort from everyone.
“It was just genuine teamwork,” Emma said.
“For example, I ended up being called up for jury duty for two weeks, so Professor Wood had to step in to take my place in the clinic and support Jon and the others. Everyone was always helping each other and going above and beyond.”
Dr Paula Lancaster, Clinical Associate Professor at the School of Dentistry, later co-authored a second paper linked to the project in the Journals of Dental Research, along with the rest of the team.
“Establishing that the more modern electric drills significantly reduced the aerosol spray was one thing, but we had another question to answer as well,” she explained.
“We needed to determine whether dentists could work safely at pre-pandemic cutting speeds of up to 200,000rpm without air coolant, or whether that might increase the risk of either or both viral aerosols and thermal damage to a tooth.”
Now requiring the real thing , Paula and the team acquired some human teeth from the School of Dentistry’s Research Tissue Bank, before using a thermal camera to identify the maximum temperature on the inside of a tooth.
This allowed them to measure the impacts of key factors such as speeds, water flow rates and different handpieces.
The reduction in aerosol spray by switching from a turbine (left) to an electric (right) handpiece
The reduction in aerosol spray by switching from a turbine (left) to an electric (right) handpiece
“What we found was that with adult teeth the risks are very low, meaning dentists can increase the RPM with confidence that they won’t cause any harm to the pulpal tissue within the centre of the tooth, while in children they should think about turning the speed down,” Paula said.
Being able to safely use higher speeds with adult patients can improve procedure efficiency, so it’s an exciting discovery.”
Making a difference in practice
The teamwork paid off.
The initial research was published in the Journal of Dental Research, with the journal’s editor praising the study for presenting a clear picture of how the risk of COVID-19 and similar hazards could be reduced with techniques set out in the team’s paper.
Jon presented the study’s findings with Professor Nattress at a meeting of the British Endodontic Society, after which he was approached by Sir Paul Beresford MP.
“Paul wanted to make sure he understood what we had found so that he could raise questions in parliament to help the government take action that would help dentistry recover after COVID-19,” Jon explained.
More recently, the team also celebrated winning one of the University’s Engaged for Impact Awards.
“We brought together a group of people with really different and varied skill sets to solve this incredibly important problem,” David said.
The result was a novel approach that is now being recognised as a gold standard.”
But it’s the difference the research could make in the real world that acts as the biggest source of the pride.
Crucially, using dental tools that produce less aerosol spray reduces the turnaround times between surgeries and can help dentists see more patients every day.
And in a country where millions haven’t had their teeth treated for years, that could make a huge difference.
About the researchers
About Emma
Emma Black is a Laboratory Manager and Senior Research Technician in Oral Biology.
Her journal articles have been published in the Journal of Pathology, the Journal of Dental Research, Cell Reports Medicine and Proceedings of the National Academy of Sciences of the United States of America, among others.
About Louise
Dr Louise Fletcher is a Lecturer in Environmental Engineering in the School of Civil Engineering.
She is interested in a range of different areas of microbiology and aerobiology, with a current focus on the generation and control of pathogens in indoor and outdoor environments.
Louise obtained her PhD in Wastewater Treatment at Leeds, as well as her MSc in Environmental Pollution Control, after completing a Geography BSc at the University of Huddersfield.
About Paula
Dr Paula Lancaster is a Clinical Associate Professor at the School of Dentistry, with expertise in restorative dentistry. She obtained her PhD using thermal imaging to assess tooth vitality.
Paula’s journal articles have been published in Frontiers of Physiology, the British Dental Journal, and the European Journal of Prosthodontics and Restorative Dentistry.
About Brian
Professor Brian Nattress is Clinical Professor/Honorary Consultant in Restorative Dentistry in the School of Dentistry, and Clinical Lead at the Translational Research Unit.
His primary research theme is clinical and applied advanced restorative dentistry.
Brian graduated from the University’s Dental School in 1980, returning to Leeds to take up the position of Lecturer in Conservative Dentistry before being appointed as a Professor in Restorative Dentistry.
About Jon
Dr Jon Vernon is a Research Fellow whose research interests include oral microbiology, dental aerosols, peri-implantitis and antimicrobial resistance.
He completed his PhD in C. difficile multi-drug resistance, bacterial fitness and mutability at Leeds, having graduated from the University of Lincoln with honours in BSc Forensic Science.
About David
Professor David Wood is the School of Dentistry’s former Director of Research and Innovation.
His research interests include natural polymer hydrogels and fibrous materials for medical and dental applications, including wound dressings, guided bone regeneration membranes and ‘smart’ vehicles for diagnosis and treatment.