Cutting out gas to make safe operations affordable and accessible
In the UK, it’s easy to take surgery for granted as something we should all be able to access when we need it. But some procedures considered everyday here are often made difficult or even impossible in many places around the world – something Professor Peter Culmer and colleagues are working hard to change.
When he was young, Peter enjoyed the kind of play that many engineers look back on fondly later in life.
“I liked making things out of wood or Lego, taking stuff apart – not that I would always put them back together again,” he recalled.
“I had that curiosity about how things operate, that desire to get creative.”
In our Further Together stories, we regularly hear how the pioneers at Leeds today knew precisely what they wanted as a career from an early age.
But with Peter, that was never the case.
“At undergraduate level I studied the very cliched combination of Maths, Physics and Chemistry before going to do an MEng in Mechatronics, but I was learning all the tools without any particular future application in mind,” he explained.
And when a lecturer mentioned an opportunity for a PhD, Peter was sceptical.
“It caught me by surprise. I didn’t think I was the kind of person who would do a PhD and was expecting some sort of career in industry instead,” he said.
“So I went along to learn more and basically rule it out.”
Only, Peter didn’t turn down the opportunity.
Instead, that PhD led to the career he’s forged now, helping medical professionals in countries with fewer healthcare resources to improve patient outcomes.
“It was quite unusual for the time because of how multidisciplinary it was,” Professor Culmer remembers.
“As well as me, there was an engineer (Dr Andrew Jackson) and a medical professional (the late Emeritus Professor Bipin Bhakta), who were working with Professor Martin Levesley and peers from outside Leeds on rehabilitation.”
The project focused on applying engineering to help stroke victims recover by developing a controller for a robotic system called iPAM that helps patients rebuild their arm, forearm and hand strength through rehab exercises.
It captured Peter’s imagination and changed his plans for the future.
The problems – and opportunities

After a few years working on the iPAM project, Peter decided to focus on healthcare more broadly.
At this time, the Leeds-based National Institute for Health Research’s (NIHR) Global Health Research Group – Surgical Technologies was working with Dr Jesudian Gnanaraj from Karunya University in Coimbatore.
Their project looked at the training in keyhole surgery that was delivered to surgeons in the rural northeast of India.
Keyhole surgery, or laparoscopy, is performed on a regular basis worldwide.
But almost a third of the 15 million operations carried out worldwide each year take place in the US alone, reflecting an eye-opening healthcare inequality: people who do not live in advanced economies are more likely to experience larger cuts, more pain, higher risks of infection and longer recoveries.
The work by the NIHR and Dr Gnanaraj highlighted a need for improved devices for this alternative type of surgery, so a partnership with Peter and his colleagues at the University of Leeds was quickly arranged.
Unequal access to keyhole surgery existed because laparoscopy comes with greater expense to hospitals and patients, takes longer and is more technically demanding than open surgery – with the need for gas, specifically carbon dioxide, a huge barrier in lower-income nations.
It’s used to inflate the patient’s abdomen and create more space for easier visibility and movement, but crucially requires theatres with a reliable CO₂ supply.
The pioneering gasless approach adopted by Dr Gnanaraj and his colleagues overcame this issue, but they were using cumbersome equipment that was hard to sterilise and maintain.
That’s the thing that motivates me, you know? Can you make an impact in the real world? That’s what makes it really exciting.”
Always taking feedback on board

The project was hugely collaborative in nature, bringing together surgeons in both India and the UK as well as the engineers at Leeds, a product design company (Pd-m International) and a manufacturing partner in India (XLO Ortho Pvt).
But what might have seemed like a daunting communication prospect proved to be a huge advantage – especially with the unexpected challenge of a pandemic lurking just around the corner.
The team set about designing a new mechanical retractor, or clamp, that could be used to lift the abdominal wall so that the patient only requires a spinal anaesthesia – meaning no need for general anaesthetic, nor an anaesthetist to be present.
From the outset, it was clear that to develop a device that would meet the precise requirements of surgeons in rural areas, designs would have to be shared frequently with stakeholders at each stage of the project.
Peter and the team understood it was important that these surgeons felt listened to and had plenty of opportunities throughout the process to provide valued feedback.
This methodology was not without its challenges, though.
“From our perspective, the development time was quite quick, certainly for a medical device,” Professor Culmer said.
“But some of the surgeons who hadn’t been involved in equipment design before might not have seen it that way, so we made sure we kept communicating with them and explaining how the process works.”
In the end, the innovative Retractor for Abdominal Insufflation-less Surgery (RAIS) device went through five design stages before a prototype was tested.
This included refinements to reduce what Peter calls initial ‘oversimplifications’; for example, when the team learned that the surgeons wanted to be able to tilt the clamp at an angle to enjoy greater visibility, they had to go back a step to ensure more flexibility could be achieved.
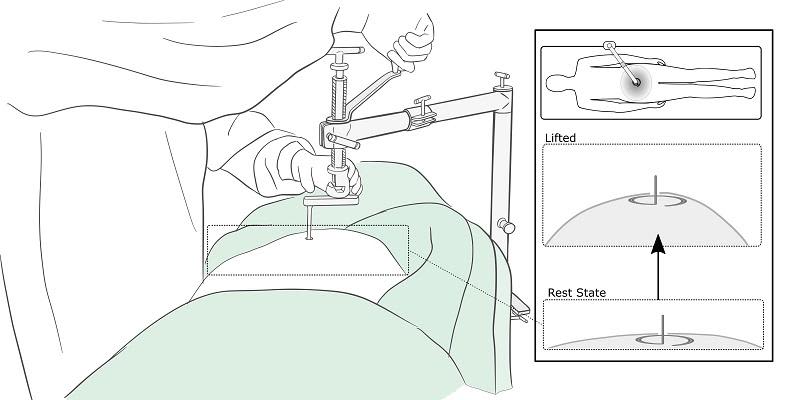
This graphic shows how the retractor works. Once in place, it is used to mechanically lift the abdominal wall, creating the necessary space for the surgeon to operate.
This graphic shows how the retractor works. Once in place, it is used to mechanically lift the abdominal wall, creating the necessary space for the surgeon to operate.
Research with global potential

After a final evaluation that had to be conducted virtually due to the pandemic, RAIS has been used in 12 laparoscopic operations, including four cases of appendicitis and two hysterectomies, with no adverse events reported.
The group’s results have been shared with policymakers and health organisations across the globe, with funding also secured to progress RAIS towards commercialisation so the training programme can be delivered to rural hospitals in Kenya.
For Peter, it’s just the start of an exciting future in which researchers in Leeds can help partners all over the world to make safe, affordable surgeries accessible to more people.
And by co-designing devices with the health professionals who will actually use them, there will be plenty of opportunities to develop transformative new equipment in the years ahead.
If you’re interested in learning more about this project including future collaboration with Peter and the team here at the University of Leeds, please email Peter at p.r.culmer@leeds.ac.uk.
About Peter
Peter Culmer is a Professor in Healthcare Technologies in the School of Mechanical Engineering at the University of Leeds.
He is also the Director of Postgraduate Research in Mechanical Engineering and sits with the IMechE's Biomedical Engineering Division (BMed).
He is the Student Summer Internships Lead and the Mechanical Engineering representative in the Robotics at Leeds network.
Peter’s technical focus is mechatronics systems for measurement and analysis of the human body, with application to medical applications including minimally invasive surgery, diabetic foot health and joint implants.